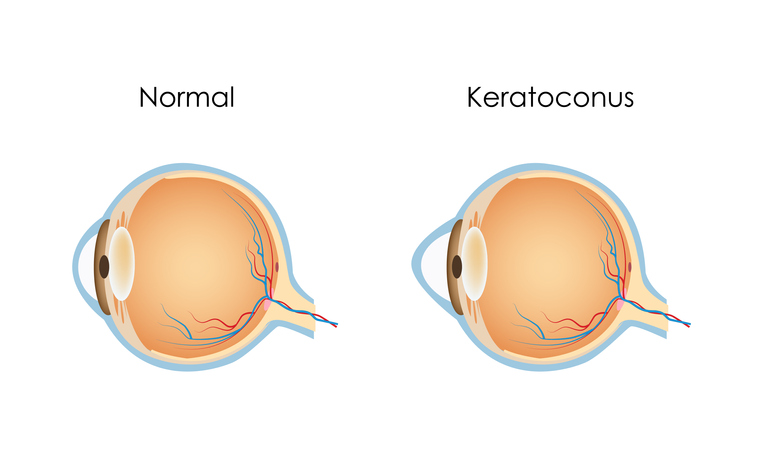
Keratoconus is a progressive condition of the eye in which the front of the eye changes shape, resembling a cone.
To understand, it helps to know a little about your corneas. Corneas are the transparent membranes in the front of your eyes, typically round. When light enters your corneas, it moves through your pupils and interior lenses and gets sent to the back of the eyes, where your retinas are.
The shape of a cornea determines how the light bounces to that retina. If a cornea is not perfectly round (often seen with nearsightedness, farsightedness, or astigmatism) it can focus the light in front of or behind the retina instead of directly to it, resulting in a blurry image instead of a clear one.
Understanding the basics of keratoconus
In keratoconus, the cornea begins to thin and develops a bulge, forming more of a front-facing cone shape instead of the normal round shape. That difference in the shape distorts the way the light refracts toward the retina, which distorts the image you see.
Keratoconus is uncommon – the Global Keratoconus Foundation estimates that somewhere between 50 to 230 people out of every 100,000 population are affected. In contrast, nearsightedness occurs in nearly 30 percent of the U.S. population. Keratoconus occurs in both sexes and all races and is found more frequently in people who have Down syndrome. It typically begins in the teenage years.
Symptoms of keratoconus
The first thing a person with developing keratoconus would notice is that their vision seems blurry even though they have seen an eye doctor for regular checkups. Typically, a keratoconus patient will experience progressive nearsightedness, often causing changes in a prescription with every visit.
They may also experience increased:
- Sensitivity to light
- Eye strain and/or general eye pain
- Glare and difficulty driving at night
- Headaches and eye irritation
Unfortunately, these symptoms can accompany other eye conditions, so it’s important to see an eye doctor. He or she will make a diagnosis based not only on symptoms but also on measurements and observation of the corneas.
Your eye doctor will use specialized tools, including a slit-lamp. This thin, focused light beam is combined with a microscope function that helps detect corneal thinning and the structure of the developing cone shape. The curvature of the cornea will be measured by how it reflects light and how its topography appears.
Treatment options for keratoconus
Depending on the severity of the condition, the following treatments can be successful:
- Eyeglasses: In the early stages of the disease, changing the prescription of your eyeglasses may be all that’s necessary. After diagnosis, your eye doctor will continue to carefully monitor further changes in your eye.
- Custom soft contact lenses: Some manufacturers have developed lenses that are customized to a wearer’s measurements and are specifically made to correct keratoconus in its mild to moderate stages.
- Rigid contact lenses: Rigid, gas-permeable lenses hold the shape of the cornea in place so that light is refracted through it correctly. They can be harder to fit and more uncomfortable to wear than soft lenses.
- “Piggybacking” contact lenses: This procedure uses both soft and rigid lenses; the soft lens is next to the eye, becoming a cushion for the harder, rigidly shaped gas-permeable contact.
- Hybrid contact lenses: The center of this contact lens is rigid, holding the cornea in place, while the outer ring of the contact is soft, providing greater comfort.
- Corneal implants: Intrastromal corneal ring segments, or Intacs, are small pieces of plastic polymer implanted in the cornea to help it hold the proper shape. The small incision heals quickly.
- Corneal transplants: About 10 to 20 percent of keratoconus patients will need a corneal transplant, in which the diseased cornea is removed from the eye and replaced with a donor cornea. Corrective eyeglasses or contact lenses may still be needed for clear vision.
- DALK transplants: Deep anterior lamellar keratoplasty (DALK) is another form of transplant, but only the front and middle layers of the cornea are transplanted; the others are still your own. Because of this, the eye heals more quickly and the likelihood of rejection is less.
What causes keratoconus?
Not only is the cause still undetermined, but the disease itself is also unpredictable – some cases will remain static in a mild state, while others continue to degenerate.
These are some of the possible factors that are involved, though it’s not clear whether the possibilities cause the keratoconus or simply take advantage of a person who has weak corneas due to the developing condition:
- Hereditary links: While there does sometimes appear to be a genetic link (in less than 10 percent of cases), most patients with keratoconus do not have any family members who have had the condition.
- Enzyme imbalances and/or oxidative stress: Recent research indicates a link between keratoconus and an imbalance of enzymes in the cornea. This could indicate a difference in how normal vs. keratoconus-affected corneas repair themselves when free-radical cells are involved.
- Eye-rubbing, allergies, and/or poorly fitting contact lenses: Excessive rubbing of the surface of the eye – whether by hand or by contact lenses that irritate the eye – has been suggested as a cause, but not proven.
- Ultraviolet exposure: The incidence of keratoconus is also associated with overexposure to ultraviolet rays from the sun.
Keratoconus is a condition that requires the expertise of a cornea specialist to diagnose and treat. Because it develops over time, it’s important to see your eye doctor for regular exams, especially if you’ve noticed any loss of clarity of vision.
Vantage Eye Center is highly invested in the health of your eyes. Contact us today with any questions on eye care or keratoconus.
Get Help Today
If symptoms of corneal diseases are uncomfortable and interfere with your daily life, call us. Our doctors have the expertise and tools to give you the relief you need.
